By QUINTON SMITH/YachatsNews.com
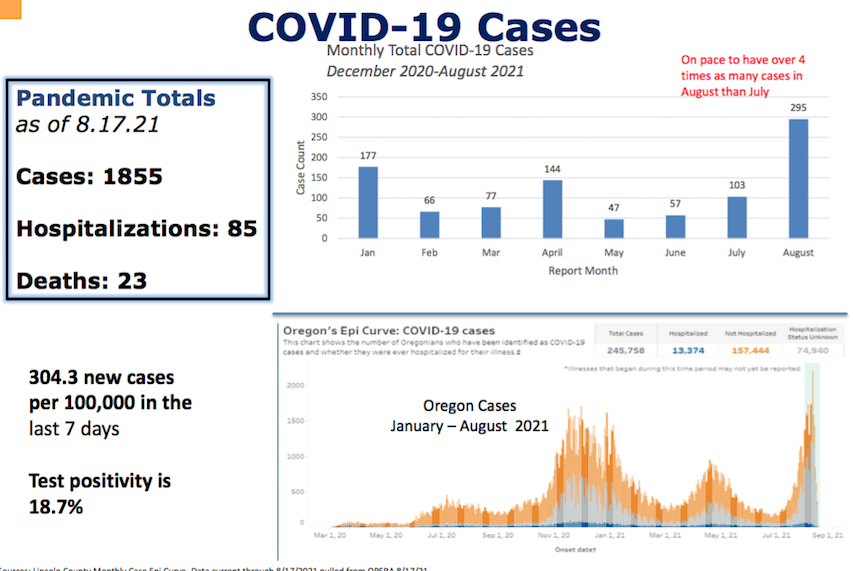
Lincoln County has had more COVID-19 cases – 422 – in the first 19 days of August than during the big Newport seafood plant outbreak last June or another spike in December.
The number includes 38 cases for Tuesday, 57 for Wednesday, and 32 Thursday and announced by the Oregon Health Authority. The 422 cases for the first three weeks of August are four times the number in all of July, when there were 103. The county had 305 in June 2020 after a big outbreak at Pacific Seafoods in Newport, and 250 cases in December during a winter surge.
But a vaccination rate of more than 75 percent – the fifth highest in Oregon – is helping prevent a rash of hospitalizations, Lincoln County interim health director Florence Pourtal told county commissioners Wednesday.
To protect themselves and others, Pourtal urged vaccine hesitant people to get the shot and for everyone to wear masks in public, indoor places and also outdoors when they could not be six feet apart.

“The Delta variant is really good at spreading fast, especially among unvaccinated populations,” Pourtal said. “Most of the people who are hospitalized at this time are not vaccinated …”
But it was the overall numbers – and a belief that many COVID-19 cases are not being reported – that worries Pourtal.
If the state was still limiting business and social activity by the number of cases in each county, Lincoln County would be in the “extreme” risk category with severe restrictions on restaurants, bars, theaters and indoor gatherings. The number of COVID-19 tests coming back positive is nearly 19 percent – almost four times the level (5 percent) at which local or state governments previously began to restrict activities.
“We have never been this high,” Pourtal said.
Other local coronavirus statistics presented Wednesday showed:
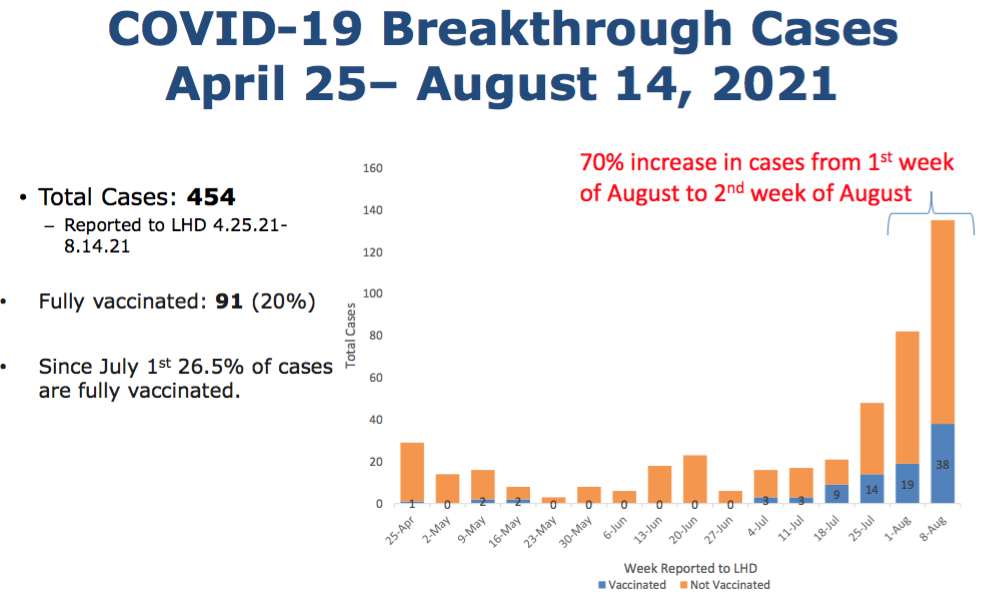
- 20 percent of hospitalizations since April were of fully vaccinated people;
- 5 percent of cases in July and August were the so-called “breakthrough” cases involving fully vaccinated people;
- The number of cases in the 0-19 age group doubled in mid-August, with children age 1-11 not being able to be vaccinated yet. “And that’s why we need to protect them,” she said.
- The most cases are now occurring in the 20-40 age group;
- There has been a “slight uptick” in the number of people getting vaccinated at mobile clinics or at summer events.
But commissioners only asked how the county can encourage more vaccinations, and asked if money or other incentives can help. They did not talk about instituting an outdoor mask mandate — as commissioners in neighboring Benton County did this week, including at Oregon State University football games in September. Benton County’s rules require anyone 5 and older to wear a mask in any outdoor, public setting where a physical distance of at least six feet cannot be maintained.
Pourtal said studies show that incentives have little effect on vaccination rates, and that the money could be better spent in other efforts – including help for a beleaguered health department staff.
Pourtal said the OHA, which has sent staff to help in the past, is already helping with three contact tracers but has no people to send to the county.
“No one was expecting for this to hit us so hard,” she said. “We can’t do it all … just want we can.”
In other Oregon, Northwest and national coronavirus news Wednesday:
- The OHA said there were 12,741 new COVID-19 cases Aug. 9-15, a 53 percent increase over the previous week, and 546 new hospitalizations, up from 224 the previous week – and the fifth consecutive week of increases;
- Oregon is now in its worst coronavirus surge since the pandemic began, The Oregonian/OregonLive reported. The state recorded the 15th highest case rate nationally over the past week, according to federal data, with parts of southern Oregon among the hardest hit in the entire country. Brown has scheduled a news conference Thursday to address the state’s response to the surge.
- Across Oregon, the OHA said only 7 percent of staffed adult hospital beds are available, and 6 percent percent of intensive care beds. In Region 2, which includes Lincoln, Benton, Linn, Marion, Polk and Yamhill counties, there were no intensive care beds empty Wednesday and only 16 out of 682 adult hospital beds available.
- Portland Public Schools, the state’s largest school district will require all of its employees to be vaccinatedagainst COVID-19 when the school year begins Sept. 1. The district said Wednesday that workers must submit proof of vaccination by the end of the month.
- Brown on Tuesday told school leaders that one of the few sure ways to keep students out of classrooms come fall is for teachers, families and school boards to defy the state’s indoor mask mandate. Brown acknowledged that Oregon’s once-solid plans to open every school for full-time in-person learning are growing less iron-clad, particularly given record transmission rates in some counties. The governor’s reprimand comes as school board meetings around the state have at times devolved into shouting matches over the governor’s July 29 order that everyone, regardless of vaccination status, must mask up inside public and private schools when classes start in the fall.
- Washington Gov. Jay Inslee announced Wednesday that all teachers and school personnel in Washington state — including coaches, bus drivers and volunteers — will need to be fully vaccinated as a condition of employment. The requirement applies to staff regardless of the type of school in which they work: public, charter or private. The policy is the strictest vaccine mandate imposed to date by any state for teachers and other staff members in schools, allowing for only a few exceptions. School staff must be vaccinated by Oct. 18 or face possible dismissal.
- Americans who received the Pfizer-BioNTech or Moderna coronavirus vaccines should get a booster shot eight months after their second vaccine dose, federal health officials said Wednesday. The boosters will be available beginning Sept. 20, if the Food and Drug Administration agrees to the plan. They will go first to health care workers, nursing home residents and older adults, who were the first to receive the initial round of vaccinations after they were authorized in December. The recommendation does not yet apply to the nearly 14 million Americans who received the single-shot Johnson & Johnson vaccine.



